Is There Still a Role for Proactive Therapeutic Drug Monitoring (TDM) in Inflammatory Bowel Disease (IBD): A Review of the Literature
DOI:
https://doi.org/10.58931/cibdt.2025.3142Abstract
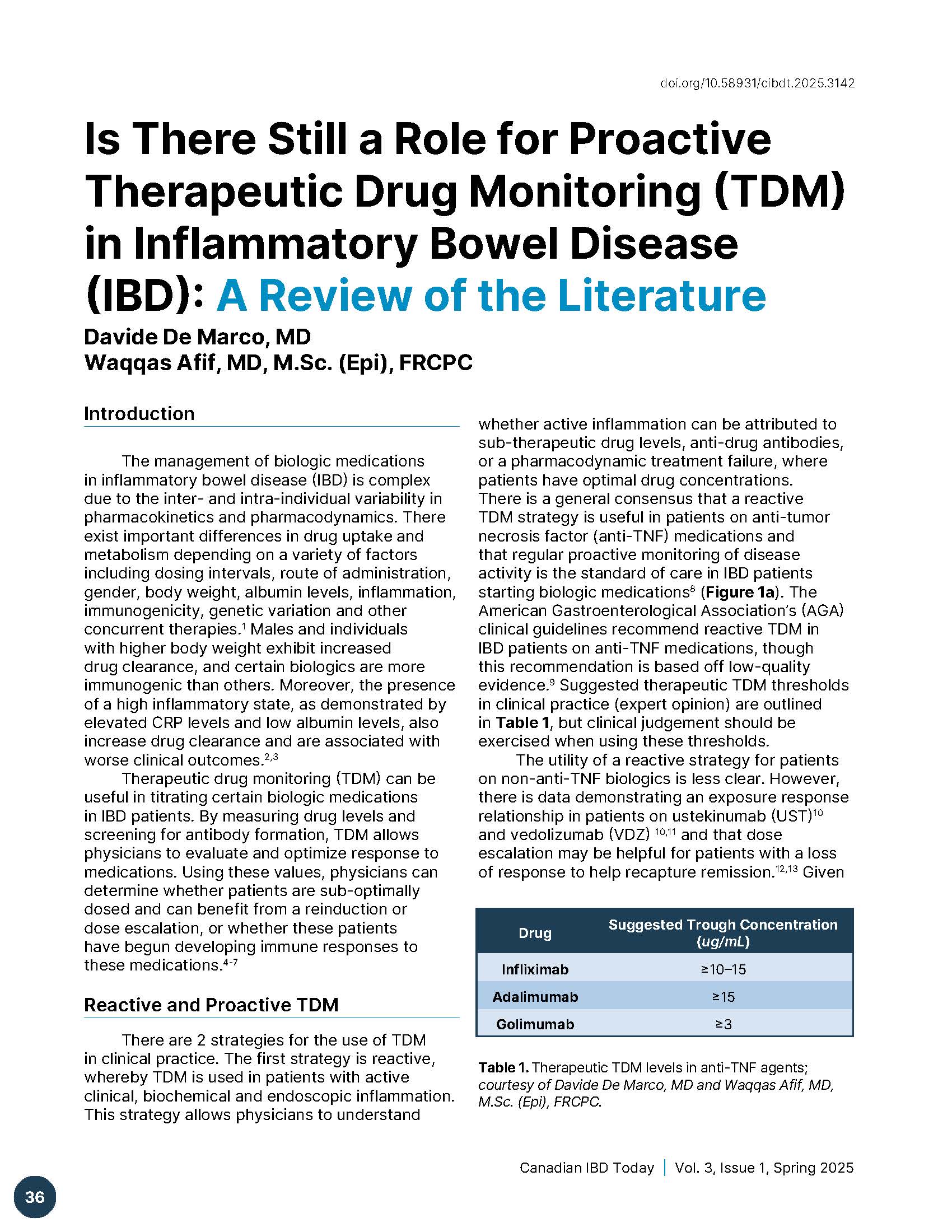
The management of biologic medications in inflammatory bowel disease (IBD) is complex due to the inter- and intra-individual variability in pharmacokinetics and pharmacodynamics. There exist important differences in drug uptake and metabolism depending on a variety of factors including dosing intervals, route of administration, gender, body weight, albumin levels, inflammation, immunogenicity, genetic variation and other concurrent therapies. Males and individuals with higher body weight exhibit increased drug clearance, and certain biologics are more immunogenic than others. Moreover, the presence of a high inflammatory state, as demonstrated by elevated CRP levels and low albumin levels, also increase drug clearance and are associated with worse clinical outcomes.
Therapeutic drug monitoring (TDM) can be useful in titrating certain biologic medications in IBD patients. By measuring drug levels and screening for antibody formation, TDM allows physicians to evaluate and optimize response to medications. Using these values, physicians can determine whether patients are sub-optimally dosed and can benefit from a reinduction or dose escalation, or whether these patients have begun developing immune responses to these medications.
References
Lefevre PL, Shackelton LM, Vande Casteele N. Factors influencing drug disposition of monoclonal antibodies in inflammatory bowel disease: implications for personalized medicine. BioDrugs. 2019;33(5):453-68. DOI: https://doi.org/10.1007/s40259-019-00366-1
Fasanmade AA, Adedokun OJ, Ford J, Hernandez D, Johanns J, Hu C, et al. Population pharmacokinetic analysis of infliximab in patients with ulcerative colitis. European journal of clinical pharmacology. 2009;65:1211-28. DOI: https://doi.org/10.1007/s00228-009-0718-4
Ordás I, Mould DR, Feagan BG, Sandborn WJ. Anti‐TNF monoclonal antibodies in inflammatory bowel disease: pharmacokinetics‐based dosing paradigms. Clinical Pharmacology & Therapeutics. 2012;91(4):635-46. DOI: https://doi.org/10.1038/clpt.2011.328
Kennedy NA, Heap GA, Green HD, Hamilton B, Bewshea C, Walker GJ, et al. Predictors of anti-TNF treatment failure in anti-TNF-naive patients with active luminal Crohn’s disease: a prospective, multicentre, cohort study. The lancet Gastroenterology & hepatology. 2019;4(5):341-53. DOI: https://doi.org/10.1016/S2468-1253(19)30012-3
Papamichael K, Cheifetz AS, Melmed GY, Irving PM, Casteele NV, Kozuch PL, et al. Appropriate therapeutic drug monitoring of biologic agents for patients with inflammatory bowel diseases. Clinical Gastroenterology and Hepatology. 2019;17(9):1655-68. e3. DOI: https://doi.org/10.1016/j.cgh.2019.03.037
Shukla R, Ananthakrishnan A. Therapeutic drug monitoring of non-anti-tumor necrosis factor biologics. Clinical Gastroenterology and Hepatology. 2021;19(6):1108-10. DOI: https://doi.org/10.1016/j.cgh.2021.01.002
Papamichael K, Afif W, Drobne D, Dubinsky MC, Ferrante M, Irving PM, et al. Therapeutic drug monitoring of biologics in inflammatory bowel disease: unmet needs and future perspectives. The lancet Gastroenterology & hepatology. 2022;7(2):171-85. DOI: https://doi.org/10.1016/S2468-1253(21)00223-5
Colombel J-F, Panaccione R, Bossuyt P, Lukas M, Baert F, Vaňásek T, et al. Effect of tight control management on Crohn’s disease (CALM): a multicentre, randomised, controlled phase 3 trial. The Lancet. 2017;390(10114):2779-89. DOI: https://doi.org/10.1016/S0140-6736(17)32641-7
Feuerstein JD, Nguyen GC, Kupfer SS, Falck-Ytter Y, Singh S, Gerson L, et al. American Gastroenterological Association Institute guideline on therapeutic drug monitoring in inflammatory bowel disease. Gastroenterology. 2017;153(3):827-34. DOI: https://doi.org/10.1053/j.gastro.2017.07.032
Singh S, Dulai PS, Vande Casteele N, Battat R, Fumery M, Boland BS, et al. Systematic review with meta‐analysis: association between vedolizumab trough concentration and clinical outcomes in patients with inflammatory bowel diseases. Alimentary pharmacology & therapeutics. 2019;50(8):848-57. DOI: https://doi.org/10.1111/apt.15484
Casteele NV, Herfarth H, Katz J, Falck-Ytter Y, Singh S. American Gastroenterological Association Institute technical review on the role of therapeutic drug monitoring in the management of inflammatory bowel diseases. Gastroenterology. 2017;153(3):835-57. e6. DOI: https://doi.org/10.1053/j.gastro.2017.07.031
Meserve J, Ma C, Dulai PS, Jairath V, Singh S. Effectiveness of reinduction and/or dose escalation of ustekinumab in Crohn’s disease: a systematic review and meta-analysis. Clinical Gastroenterology and Hepatology. 2022;20(12):2728-40. e1. DOI: https://doi.org/10.1016/j.cgh.2021.10.002
Peyrin-Biroulet L, Danese S, Argollo M, Pouillon L, Peppas S, Gonzalez-Lorenzo M, et al. Loss of response to vedolizumab and ability of dose intensification to restore response in patients with Crohn’s disease or ulcerative colitis: a systematic review and meta-analysis. Clinical Gastroenterology and Hepatology. 2019;17(5):838-46. e2. DOI: https://doi.org/10.1016/j.cgh.2018.06.026
Sandborn WJ, Su C, Sands BE, D’Haens GR, Vermeire S, Schreiber S, et al. Tofacitinib as induction and maintenance therapy for ulcerative colitis. New England Journal of Medicine. 2017;376(18):1723-36. DOI: https://doi.org/10.1056/NEJMoa1606910
Sandborn WJ, Peyrin-Biroulet L, Sharara AI, Su C, Modesto I, Mundayat R, et al. Efficacy and safety of tofacitinib in ulcerative colitis based on prior tumor necrosis factor inhibitor failure status. Clinical Gastroenterology and Hepatology. 2022;20(3):591-601. e8. DOI: https://doi.org/10.1016/j.cgh.2021.02.043
Muensterman E, Engelhardt B, Gopalakrishnan S, Anderson JK, Mohamed MEF. Upadacitinib pharmacokinetics and exposure‐response analyses of efficacy and safety in psoriatic arthritis patients–Analyses of phase III clinical trials. Clinical and Translational Science. 2022;15(1):267-78. DOI: https://doi.org/10.1111/cts.13146
Ponce-Bobadilla AV, Stodtmann S, Eckert D, Zhou W, Liu W, Mohamed M-EF. Upadacitinib population pharmacokinetics and exposure-response relationships in ulcerative colitis patients. Clinical Pharmacokinetics. 2023;62(1):101-12. DOI: https://doi.org/10.1007/s40262-022-01191-6
Danese S, Vermeire S, Zhou W, Pangan AL, Siffledeen J, Greenbloom S, et al. Upadacitinib as induction and maintenance therapy for moderately to severely active ulcerative colitis: results from three phase 3, multicentre, double-blind, randomised trials. The lancet. 2022;399(10341):2113-28. DOI: https://doi.org/10.1016/S0140-6736(22)00581-5
Loftus Jr EV, Panés J, Lacerda AP, Peyrin-Biroulet L, D’Haens G, Panaccione R, et al. Upadacitinib induction and maintenance therapy for Crohn’s disease. New England Journal of Medicine. 2023;388(21):1966-80. DOI: https://doi.org/10.1056/NEJMoa2212728
Sandborn WJ, Feagan BG, D’Haens G, Wolf DC, Jovanovic I, Hanauer SB, et al. Ozanimod as induction and maintenance therapy for ulcerative colitis. New England Journal of Medicine. 2021;385(14):1280-91. DOI: https://doi.org/10.1056/NEJMoa2033617
Sands BE, Schreiber S, Blumenstein I, Chiorean MV, Ungaro RC, Rubin DT. Clinician’s guide to using ozanimod for the treatment of ulcerative colitis. Journal of Crohn’s and Colitis. 2023;17(12):2012-25. DOI: https://doi.org/10.1093/ecco-jcc/jjad112
Sethi S, Dias S, Kumar A, Blackwell J, Brookes MJ, Segal JP. Meta‐analysis: The efficacy of therapeutic drug monitoring of anti‐TNF‐therapy in inflammatory bowel disease. Alimentary Pharmacology & Therapeutics. 2023;57(12):1362-74. DOI: https://doi.org/10.1111/apt.17313
Nguyen NH, Solitano V, Vuyyuru SK, MacDonald JK, Syversen SW, Jørgensen KK, et al. Proactive therapeutic drug monitoring versus conventional management for inflammatory bowel diseases: a systematic review and meta-analysis. Gastroenterology. 2022;163(4):937-49. e2. DOI: https://doi.org/10.1053/j.gastro.2022.06.052
Peyrin–Biroulet L, Deltenre P, De Suray N, Branche J, Sandborn WJ, Colombel JF. Efficacy and safety of tumor necrosis factor antagonists in Crohn’s disease: meta-analysis of placebo-controlled trials. Clinical Gastroenterology and Hepatology. 2008;6(6):644-53. DOI: https://doi.org/10.1016/j.cgh.2008.03.014
Lv R, Qiao W, Wu Z, Wang Y, Dai S, Liu Q, et al. Tumor necrosis factor alpha blocking agents as treatment for ulcerative colitis intolerant or refractory to conventional medical therapy: a meta-analysis. PloS one. 2014;9(1):e86692. DOI: https://doi.org/10.1371/journal.pone.0086692
Hanauer SB, Feagan BG, Lichtenstein GR, Mayer LF, Schreiber S, Colombel JF, et al. Maintenance infliximab for Crohn’s disease: the ACCENT I randomised trial. The Lancet. 2002;359(9317):1541-9. DOI: https://doi.org/10.1016/S0140-6736(02)08512-4
Hanauer SB, Sandborn WJ, Rutgeerts P, Fedorak RN, Lukas M, MacIntosh D, et al. Human anti–tumor necrosis factor monoclonal antibody (adalimumab) in Crohn’s disease: the CLASSIC-I Trial. Gastroenterology. 2006;130(2):323-33. DOI: https://doi.org/10.1053/j.gastro.2005.11.030
Colombel JF, Sandborn WJ, Rutgeerts P, Enns R, Hanauer SB, Panaccione R, et al. Adalimumab for maintenance of clinical response and remission in patients with Crohn’s disease: the CHARM trial. Gastroenterology. 2007;132(1):52-65. DOI: https://doi.org/10.1053/j.gastro.2006.11.041
Reinisch W, Sandborn WJ, Rutgeerts P, Feagan BG, Rachmilewitz D, Hanauer SB, et al. Long-term infliximab maintenance therapy for ulcerative colitis: the ACT-1 and-2 extension studies. Inflammatory bowel diseases. 2012;18(2):201-11. DOI: https://doi.org/10.1002/ibd.21697
Colombel JF, Sandborn WJ, Reinisch W, Mantzaris GJ, Kornbluth A, Rachmilewitz D, et al. Infliximab, azathioprine, or combination therapy for Crohn’s disease. New England journal of medicine. 2010;362(15):1383-95. DOI: https://doi.org/10.1056/NEJMoa0904492
Seow CH, Newman A, Irwin SP, Steinhart AH, Silverberg MS, Greenberg GR. Trough serum infliximab: a predictive factor of clinical outcome for infliximab treatment in acute ulcerative colitis. Gut. 2010;59(01):49-54. DOI: https://doi.org/10.1136/gut.2009.183095
Maser EA, Villela R, Silverberg MS, Greenberg GR. Association of trough serum infliximab to clinical outcome after scheduled maintenance treatment for Crohn’s disease. Clinical Gastroenterology and Hepatology. 2006;4(10):1248-54. DOI: https://doi.org/10.1016/j.cgh.2006.06.025
Adedokun OJ, Sandborn WJ, Feagan BG, Rutgeerts P, Xu Z, Marano CW, et al. Association between serum concentration of infliximab and efficacy in adult patients with ulcerative colitis. Gastroenterology. 2014;147(6):1296-307. e5. DOI: https://doi.org/10.1053/j.gastro.2014.08.035
Cornillie F, Hanauer SB, Diamond RH, Wang J, Tang KL, Xu Z, et al. Postinduction serum infliximab trough level and decrease of C-reactive protein level are associated with durable sustained response to infliximab: a retrospective analysis of the ACCENT I trial. Gut. 2014;63(11):1721-7. DOI: https://doi.org/10.1136/gutjnl-2012-304094
Papamichael K, Gils A, Rutgeerts P, Levesque BG, Vermeire S, Sandborn WJ, et al. Role for therapeutic drug monitoring during induction therapy with TNF antagonists in IBD: evolution in the definition and management of primary nonresponse. Inflammatory bowel diseases. 2015;21(1):182-97. DOI: https://doi.org/10.1097/MIB.0000000000000202
Vande Casteele N, Papamichael K, Jeyarajah J, Osterman M, Cheifetz A. DOP45 Adequate infliximab exposure during the induction phase is associated with early complete fistula response in patients with fistulizing Crohn’s disease: a post-hoc analysis of the ACCENT-2 trial. Journal of Crohn’s and Colitis. 2019;13(Supplement_1):S053-S4. DOI: https://doi.org/10.1093/ecco-jcc/jjy222.079
Battat R, Lukin D, Scherl EJ, Pola S, Kumar A, Okada L, et al. Immunogenicity of tumor necrosis factor antagonists and effect of dose escalation on anti-drug antibodies and serum drug concentrations in inflammatory bowel disease. Inflammatory bowel diseases. 2021;27(9):1443-51. DOI: https://doi.org/10.1093/ibd/izaa313
Casteele NV, Ferrante M, Van Assche G, Ballet V, Compernolle G, Van Steen K, et al. Trough concentrations of infliximab guide dosing for patients with inflammatory bowel disease. Gastroenterology. 2015;148(7):1320-9. e3. DOI: https://doi.org/10.1053/j.gastro.2015.02.031
D’Haens G, Vermeire S, Lambrecht G, Baert F, Bossuyt P, Pariente B, et al. Increasing infliximab dose based on symptoms, biomarkers, and serum drug concentrations does not increase clinical, endoscopic, and corticosteroid-free remission in patients with active luminal Crohn’s disease. Gastroenterology. 2018;154(5):1343-51. e1. DOI: https://doi.org/10.1053/j.gastro.2018.01.004
Assa A, Matar M, Turner D, Broide E, Weiss B, Ledder O, et al. Proactive monitoring of adalimumab trough concentration associated with increased clinical remission in children with Crohn’s disease compared with reactive monitoring. Gastroenterology. 2019;157(4):985-96. e2. DOI: https://doi.org/10.1053/j.gastro.2019.06.003
Seow CH, Marshall JK, Stewart E, Pettengell C, Ward R, Afif W. The relationship among vedolizumab drug concentrations, biomarkers of inflammation, and clinical outcomes in a Canadian real-world study. Journal of the Canadian Association of Gastroenterology. 2024;7(4):290-8. DOI: https://doi.org/10.1093/jcag/gwae010
Porth R, Deyhim T, Zullow S, Rabinowitz LG, Grossberg LB, Roblin X, et al. Proactive therapeutic drug monitoring is associated with increased drug persistence in patients with inflammatory bowel disease treated with intravenous vedolizumab. Inflammatory Bowel Diseases. 2024:izae140.
Jairath V, Yarur A, Osterman MT, James A, Balma D, Mehrotra S, et al. ENTERPRET: a randomized controlled trial of vedolizumab dose optimization in patients with ulcerative colitis who have early nonresponse. Clinical Gastroenterology and Hepatology. 2024;22(5):1077-86. e13. DOI: https://doi.org/10.1016/j.cgh.2023.10.029
Porth R, Deyhim T, Geeganage G, Smith B, Zullow S, Rabinowitz LG, et al. Proactive Therapeutic Drug Monitoring of Ustekinumab Is Associated With Increased Drug Persistence in Patients With Inflammatory Bowel Disease. Inflammatory Bowel Diseases. 2024:izae231. DOI: https://doi.org/10.1093/ibd/izae231
Wang Z, Hoffert Y, Zhang W, Kantasiripitak W, Verstockt B, Sabino J, et al. OP12 Therapeutic antibody clearance better predicts endoscopic outcomes than trough concentrations in patients with Crohn’s disease. Journal of Crohn’s and Colitis. 2025;19(Supplement_1):i24-i6. DOI: https://doi.org/10.1093/ecco-jcc/jjae190.0012
Wu J-F. Therapeutic drug monitoring of biologics for patients with inflammatory bowel diseases: how, when, and for whom? Gut and Liver. 2021;16(4):515. DOI: https://doi.org/10.5009/gnl210262
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Canadian IBD Today

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
