Practical Approach to Abnormal Liver Enzymes in Patients with Inflammatory Bowel Disease
DOI:
https://doi.org/10.58931/cibdt.2023.1317Abstract
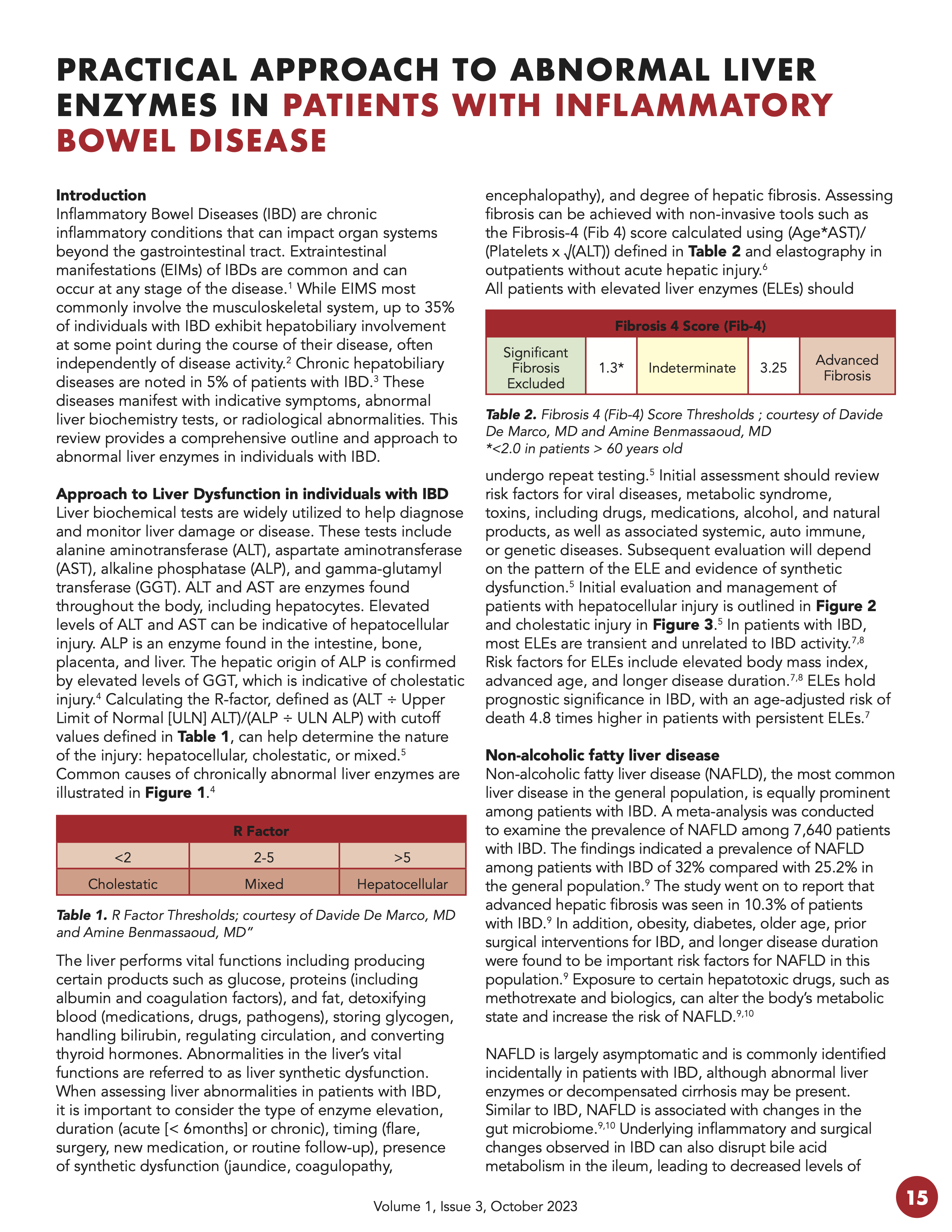
Inflammatory Bowel Diseases (IBD) are chronic inflammatory conditions that can impact organ systems beyond the gastrointestinal tract. Extraintestinal manifestations (EIMs) of IBDs are common and can occur at any stage of the disease. While EIMS most commonly involve the musculoskeletal system, up to 35% of individuals with IBD exhibit hepatobiliary involvement at some point during the course of their disease, often independently of disease activity. Chronic hepatobiliary diseases are noted in 5% of patients with IBD. These diseases manifest with indicative symptoms, abnormal liver biochemistry tests, or radiological abnormalities. This review provides a comprehensive outline and approach to abnormal liver enzymes in individuals with IBD.
References
Rogler G, Singh A, Kavanaugh A, Rubin DT. Extraintestinal manifestations of inflammatory bowel disease: current concepts, treatment, and implications for disease management. Gastroenterology. 2021;161(4):1118-32. doi: 10.1053/j.gastro.2021.07.042 DOI: https://doi.org/10.1053/j.gastro.2021.07.042
Vavricka SR, Schoepfer A, Scharl M, Lakatos PL, Navarini A, Rogler G. Extraintestinal manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2015;21(8):1982-92. doi: 10.1097/MIB.0000000000000392 DOI: https://doi.org/10.1097/MIB.0000000000000392
Mendes FD, Levy C, Enders FB, Loftus EV Jr, Angulo P, Lindor KD. Abnormal hepatic biochemistries in patients with inflammatory bowel disease. Am J Gastroenterol. 2007;102(2):344-50. doi: 10.1111/j.1572-0241.2006.00947.x DOI: https://doi.org/10.1111/j.1572-0241.2006.00947.x
Kalas MA, Chavez L, Leon M, Taweesedt PT, Surani S. Abnormal liver enzymes: a review for clinicians. World J Hepatol. 2021;13(11):1688-98. doi: 10.4254/wjh.v13.i11.1688 DOI: https://doi.org/10.4254/wjh.v13.i11.1688
Kwo PY, Cohen SM, Lim JK. ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries. Am J Gastroenerol. 2017;112(1):18-35. doi: 10.1038/ajg.2016.517. DOI: https://doi.org/10.1038/ajg.2016.517
European Association for the Study of the Liver. EASL Clinical Practice Guidelines on non-invasive tests for evaluation of liver disease severity and prognosis–2021 update. J Hepatol. 2021;75(3):659-89. doi: 10.1016/j.jhep.2021.05.025 DOI: https://doi.org/10.1016/j.jhep.2021.05.025
Cheng YW, McLean R, Sewell JL, Huang CY, Khalili M. Inflammatory bowel disease type influences development of elevated liver enzymes. JGH Open. 2022;6(12):846-53. doi: 10.1002/jgh3.12831 DOI: https://doi.org/10.1002/jgh3.12831
Cappello M, Randazzo C, Bravatà I, Licata A, Peralta S, Craxì A, et al. Liver function test abnormalities in patients with inflammatory bowel diseases: a hospital-based survey. Clin Med Insights Gastroenterol. 2014;7:25-31. doi: 10.4137/CGast.S13125. DOI: https://doi.org/10.4137/CGast.S13125
Lin A, Roth H, Anyane-Yeboa A, Rubin DT, Paul S. Prevalence of nonalcoholic fatty liver disease in patients with inflammatory bowel disease: a systematic review and meta-analysis. Inflamm Bowel Dis. 2020;27(6):947-55. doi: 10.1093/ibd/izaa189 DOI: https://doi.org/10.1093/ibd/izaa189
Bessissow T, Le NH, Rollet K, Afif W, Bitton A, Sebastiani G. Incidence and predictors of nonalcoholic fatty liver disease by serum biomarkers in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2016;22(8):1937-44. doi: 10.1097/MIB.0000000000000832 DOI: https://doi.org/10.1097/MIB.0000000000000832
Mancina RM, Spagnuolo R, Milano M, Brogneri S, Morrone A, Cosco C, et al. PNPLA3 148M carriers with inflammatory bowel diseases have higher susceptibility to hepatic steatosis and higher liver enzymes. Inflamm Bowel Dis. 2016;22(1):134-40. doi: 10.1097/MIB.0000000000000569 DOI: https://doi.org/10.1097/MIB.0000000000000569
Newsome PN, Cramb R, Davison SM, Dillon JF, Foulerton M, Godfrey EM, et al. Guidelines on the management of abnormal liver blood tests. Gut. 2018;67(1):6-19. doi: 10.1136/gutjnl-2017-314924 DOI: https://doi.org/10.1136/gutjnl-2017-314924
Rinella ME, Neuschwander-Tetri BA, Siddiqui MS, Abdelmalek MF, Caldwell S, Barb D, et al. AASLD Practice Guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology. 2023;77(5):1797-835. doi: 10.1097/HEP.0000000000000323 DOI: https://doi.org/10.1097/HEP.0000000000000323
Saroli Palumbo C, Restellini S, Chao C-Y, Aruljothy A, Lemieux C, Wild G, et al. Screening for nonalcoholic fatty liver disease in inflammatory bowel diseases: a cohort study using transient elastography. Inflamm Bowel Dis. 2018;25(1):124-33. doi: 10.1093/ibd/izy200 DOI: https://doi.org/10.1093/ibd/izy200
Barberio B, Massimi D, Cazzagon N, Zingone F, Ford AC, Savarino EV. Prevalence of primary sclerosing cholangitis in patients with inflammatory bowel disease: a systematic review and meta-analysis. Gastroenterology. 2021;161(6):1865-77. doi: 10.1053/j.gastro.2021.08.032 DOI: https://doi.org/10.1053/j.gastro.2021.08.032
Lunder AK, Hov JR, Borthne A, Gleditsch J, Johannesen G, Tveit K, et al. Prevalence of sclerosing cholangitis detected by magnetic resonance cholangiography in patients with long-term inflammatory bowel disease. Gastroenterology. 2016;151(4):660-9. e4. doi: 10.1053/j.gastro.2016.06.021 DOI: https://doi.org/10.1053/j.gastro.2016.06.021
Saich R, Chapman R. Primary sclerosing cholangitis, autoimmune hepatitis and overlap syndromes in inflammatory bowel disease. World J Gastroenterol. 2008;14(3):331-7. doi: 10.3748/wjg.14.331 DOI: https://doi.org/10.3748/wjg.14.331
Bowlus CL, Arrivé L, Bergquist A, Deneau M, Forman L, Ilyas SI, et al. AASLD practice guidance on primary sclerosing cholangitis and cholangiocarcinoma. Hepatology. 2023;77(2):659-702. doi: 10.1002/hep.32771 DOI: https://doi.org/10.1002/hep.32771
Soetikno RM, Lin OS, Heidenreich PA, Young HS, Blackstone MO. Increased risk of colorectal neoplasia in patients with primary sclerosing cholangitis and ulcerative colitis: a meta-analysis. Gastrointest Endosc. 2002;56(1):48-54. doi: 10.1067/mge.2002.125367 DOI: https://doi.org/10.1067/mge.2002.125367
Janse M, Lamberts LE, Franke L, Raychaudhuri S, Ellinghaus E, Muri Boberg K, et al. Three ulcerative colitis susceptibility loci are associated with primary sclerosing cholangitis and indicate a role for IL2, REL, and CARD9. Hepatology. 2011;53(6):1977-85. doi: 10.1002/hep.24307 DOI: https://doi.org/10.1002/hep.24307
European Association for the Study of the Liver. EASL Clinical Practice Guidelines on sclerosing cholangitis. J Hepatol. 2022;77(3):761-806. doi: 10.1016/j.jhep.2022.05.011 DOI: https://doi.org/10.1016/j.jhep.2022.05.011
DeFilippis EM, Kumar S. Clinical presentation and outcomes of autoimmune hepatitis in inflammatory bowel disease. Dig Dis Sci. 2015;60(10):2873-80. doi: 10.1007/s10620-015-3699-4. DOI: https://doi.org/10.1007/s10620-015-3699-4
Mack CL, Adams D, Assis DN, Kerkar N, Manns MP, Mayo MJ, et al. Diagnosis and management of autoimmune hepatitis in adults and children: 2019 Practice Guidance and Guidelines From the American Association for the Study of Liver Diseases. Hepatology. 2020;72(2):671-722. doi: 10.1002/hep.31065 DOI: https://doi.org/10.1002/hep.31065
Hennes EM, Zeniya M, Czaja AJ, Parés A, Dalekos GN, Krawitt EL, et al. Simplified criteria for the diagnosis of autoimmune hepatitis. Hepatology. 2008;48(1):169-76. doi: 10.1002/hep.22322. DOI: https://doi.org/10.1002/hep.22322
Colina F, Molero A, Casís B, Martínez-Montiel P. Infliximab-related hepatitis: a case study and literature review. Dig Dis Sci. 2013;58:3362-7. doi: 10.1007/s10620-013-2698-6. DOI: https://doi.org/10.1007/s10620-013-2698-6
Grainge MJ, West J, Card TR. Venous thromboembolism during active disease and remission in inflammatory bowel disease: a cohort study. Lancet. 2010;375(9715):657-63. doi: 10.1016/S0140-6736(09)61963-2 DOI: https://doi.org/10.1016/S0140-6736(09)61963-2
Gizard E, Ford AC, Bronowicki J-P, Peyrin-Biroulet L. Systematic review: the epidemiology of the hepatobiliary manifestations in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2014;40(1):3-15. doi: 10.1111/apt.12794 DOI: https://doi.org/10.1111/apt.12794
Naymagon L, Tremblay D, Zubizarreta N, Moshier E, Naymagon S, Mascarenhas J, et al. The natural history, treatments, and outcomes of portal vein thrombosis in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2021;27(2):215-23. doi: 10.1093/ibd/izaa053 DOI: https://doi.org/10.1093/ibd/izaa053
Benmassaoud A, AlRubaiy L, Yu D, Chowdary P, Sekhar M, Parikh P, et al. A stepwise thrombolysis regimen in the management of acute portal vein thrombosis in patients with evidence of intestinal ischaemia. Aliment Pharmacol Ther. 2019;50(9):1049-58. doi: 10.1111/apt.15479 DOI: https://doi.org/10.1111/apt.15479
European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Vascular diseases of the liver. J Hepatol. 2016;64(1):179-202. DOI: https://doi.org/10.1016/j.jhep.2015.07.040
Baig MM, Irfan SA, Sumbal A, Sumbal R, Kumar S, Ahmad J, et al. Prevalence of gallstones in ulcerative colitis and crohn’s disease: a systematic review and meta-analysis. Cureus. 2022;14(6):e26121. doi: 10.7759/cureus.26121 DOI: https://doi.org/10.7759/cureus.26121
Restellini S, Chazouillères O, Frossard J-L. Hepatic manifestations of inflammatory bowel diseases. Liver Int. 2017;37(4):475-89. doi: 10.1111/liv.13265 DOI: https://doi.org/10.1111/liv.13265
Zhang FM, Xu CF, Shan GD, Chen HT, Xu GQ. Is gallstone disease associated with inflammatory bowel diseases? A meta‐analysis. J Dig Dis. 2015 Nov;16(11):634-41. doi: 10.1111/1751-2980 DOI: https://doi.org/10.1111/1751-2980.12286
Coffin CS, Fung SK, Alvarez F, Cooper CL, Doucette KE, Fournier C, et al. Management of hepatitis B virus infection: 2018 Guidelines from the Canadian Association for the Study of Liver Disease and Association of Medical Microbiology and Infectious Disease Canada. Can Liver J. 2018;1(4):156-217. doi: 10.3138/canlivj.2018-0008 DOI: https://doi.org/10.3138/canlivj.2018-0008
Núñez F P, Quera R, Bay C, Castro F, Mezzano G. Drug-induced liver injury used in the treatment of inflammatory bowel disease. J Crohns Colitis. 2022;16(7):1168-76. doi: 10.1093/ecco-jcc/jjac013 DOI: https://doi.org/10.1093/ecco-jcc/jjac013
Perrillo RP, Gish R, Falck-Ytter YT. American Gastroenterological Association Institute technical review on prevention and treatment of hepatitis B virus reactivation during immunosuppressive drug therapy. Gastroenterology. 2015;148(1):221-44. e3. doi: 10.1053/j.gastro.2014.10.038. DOI: https://doi.org/10.1053/j.gastro.2014.10.038
Rahier J-F, Ben-Horin S, Chowers Y, Conlon C, De Munter P, D'Haens G, et al. European evidence-based Consensus on the prevention, diagnosis and management of opportunistic infections in inflammatory bowel disease. J Crohns Colitis. 2009;3(2):47-91. doi: 10.1016/j.crohns.2009.02.010 DOI: https://doi.org/10.1016/j.crohns.2009.02.010
European Association for the Study of the Liver. EASL Clinical Practice Guidelines: drug-induced liver injury. J Hepatol. 2019;70(6):1222-61. doi: 10.1016/j.jhep.2019.02.014 DOI: https://doi.org/10.1016/j.jhep.2019.02.014
Hoofnagle JH. LiverTox: a website on drug-induced liver injury. In: Kaplowitz N, DeLeve LD, editors. Drug-induced liver disease 3rd ed. Elsevier; 2013. p. 725-32. DOI: https://doi.org/10.1016/B978-0-12-387817-5.00040-6
Danan G, Teschke R. RUCAM in drug and herb induced liver injury: the update. Int J Mol Sci. 2015;17(1):14. doi: 10.3390/ijms17010014 DOI: https://doi.org/10.3390/ijms17010014
Chaparro M, Ordás I, Cabré E, Garcia-Sanchez V, Bastida G, Peñalva M, et al. Safety of thiopurine therapy in inflammatory bowel disease: long-term follow-up study of 3931 patients. Inflamm Bowel Dis. 2013;19(7):1404-10. doi: 10.1097/MIB.0b013e318281f28f. DOI: https://doi.org/10.1097/MIB.0b013e318281f28f
Tominaga K, Sugaya T, Tanaka T, Kanazawa M, Iijima M, Irisawa A. Thiopurines: recent topics and their role in the treatment of inflammatory bowel diseases. Front Pharmacol. 2021;11:582291. doi: 10.3389/fphar.2020.582291 DOI: https://doi.org/10.3389/fphar.2020.582291
Gisbert JP, González-Lama Y, Maté J. Thiopurine-induced liver injury in patients with inflammatory bowel disease: a systematic review. Am J Gastroenterol. 2007;102(7):1518-27. doi: 10.1111/j.1572-0241.2007.01187.x DOI: https://doi.org/10.1111/j.1572-0241.2007.01187.x
Benmassaoud A, Xie X, AlYafi M, Theoret Y, Bitton A, Afif W, et al. Thiopurines in the management of Crohn's disease: safety and efficacy profile in patients with normal TPMT activity-a retrospective study. Can J Gastroenterol Hepatol. 2016;2016:1034834. doi: 10.1155/2016/1034834 DOI: https://doi.org/10.1155/2016/1034834
Feagan BG, Chande N, MacDonald JK. Are there any differences in the efficacy and safety of different formulations of Oral 5-ASA used for induction and maintenance of remission in ulcerative colitis? evidence from cochrane reviews. Inflamm bowel dis. 2013;19(9):2031-40. doi: 10.1097/MIB.0b013e3182920108 DOI: https://doi.org/10.1097/MIB.0b013e3182920108
Torres J, Bonovas S, Doherty G, Kucharzik T, Gisbert JP, Raine T, et al. ECCO Guidelines on Therapeutics in Crohn's Disease: medical treatment. J Crohns Colitis. 2020;14(1):4-22. doi: 10.1093/ecco-jcc/jjz180 DOI: https://doi.org/10.1093/ecco-jcc/jjz180
Saibeni S, Bollani S, Losco A, Michielan A, Sostegni R, Devani M, et al. The use of methotrexate for treatment of inflammatory bowel disease in clinical practice. Dig Liver Dis. 2012;44(2):123-7. doi: 10.1016/j.dld.2011.09.015 DOI: https://doi.org/10.1016/j.dld.2011.09.015
De Marco D, Bessissow T, Marcus V, Benmassaoud A. Vedolizumab-associated hypereosinophilia and hepatoxicity. ACG Case Rep J. 2022;9(11):e00905. doi: 10.14309/crj.0000000000000905 DOI: https://doi.org/10.14309/crj.0000000000000905
D’Amico F, Parigi TL, Fiorino G, Peyrin-Biroulet L, Danese S. Tofacitinib in the treatment of ulcerative colitis: efficacy and safety from clinical trials to real-world experience. Therap Adv Gastroenterol. 2019;12:1756284819848631. doi: 10.1177/1756284819848631 DOI: https://doi.org/10.1177/1756284819848631
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Canadian IBD Today

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
