Selective JAK1 Inhibition Using Upadacitinib for the Management of Inflammatory Bowel Diseases
The Powerful Pill
DOI:
https://doi.org/10.58931/cibdt.2023.1S1121Abstract
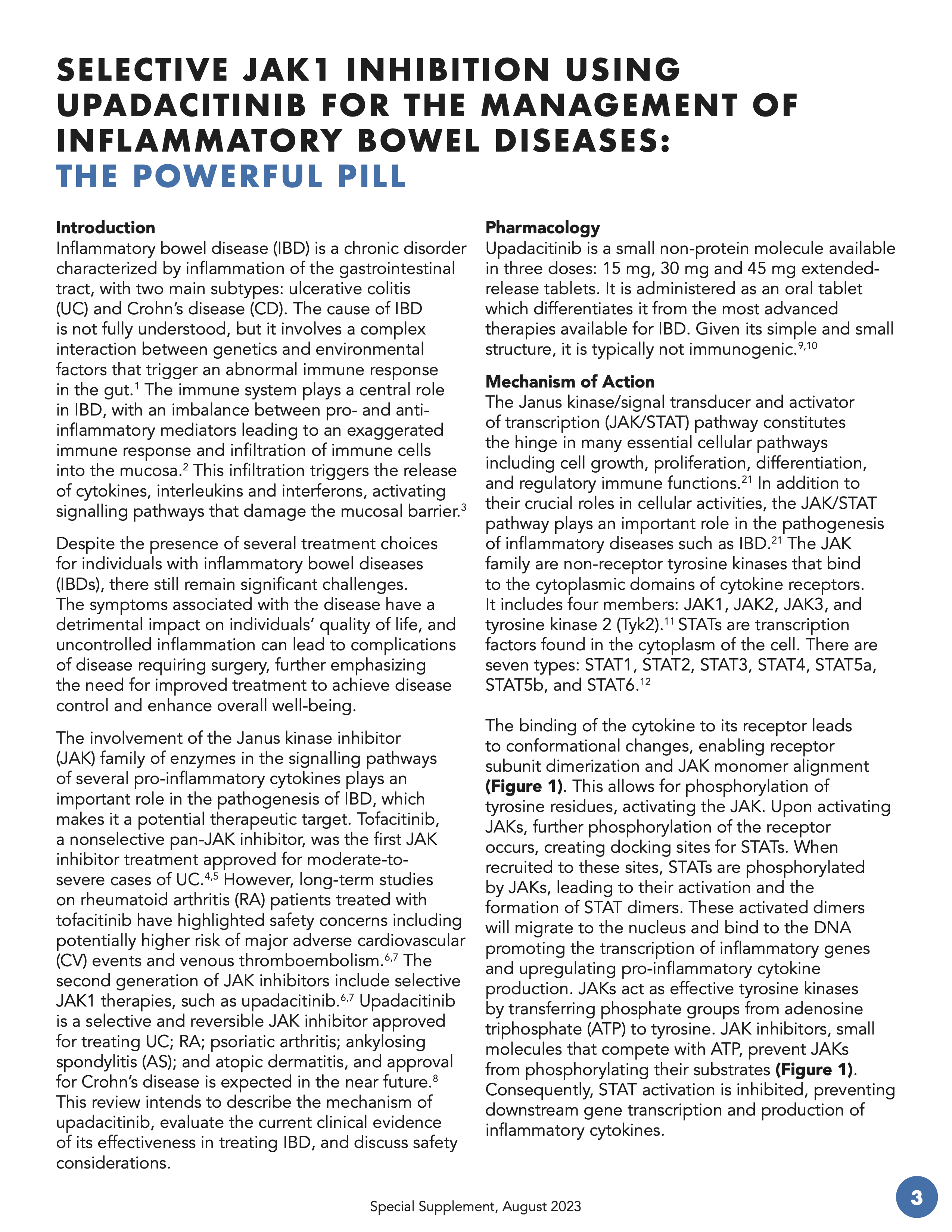
Inflammatory bowel disease (IBD) is a chronic disorder characterized by inflammation of the gastrointestinal tract, with two main subtypes: ulcerative colitis (UC) and Crohn’s disease (CD). The cause of IBD is not fully understood, but it involves a complex interaction between genetics and environmental factors that trigger an abnormal immune response in the gut. The immune system plays a central role in IBD, with an imbalance between pro- and anti-inflammatory mediators leading to an exaggerated immune response and infiltration of immune cells into the mucosa.2 This infiltration triggers the release of cytokines, interleukins and interferons, activating signalling pathways that damage the mucosal barrier.
Despite the presence of several treatment choices for individuals with inflammatory bowel diseases (IBDs), there still remain significant challenges. The symptoms associated with the disease have a detrimental impact on individuals’ quality of life, and uncontrolled inflammation can lead to complications of disease requiring surgery, further emphasizing the need for improved treatment to achieve disease control and enhance overall well-being.
The involvement of the Janus kinase inhibitor (JAK) family of enzymes in the signalling pathways of several pro-inflammatory cytokines plays an important role in the pathogenesis of IBD, which makes it a potential therapeutic target. Tofacitinib, a nonselective pan-JAK inhibitor, was the first JAK inhibitor treatment approved for moderate-to-severe cases of UC. However, long-term studies on rheumatoid arthritis (RA) patients treated with tofacitinib have highlighted safety concerns including potentially higher risk of major adverse cardiovascular (CV) events and venous thromboembolism. The second generation of JAK inhibitors include selective JAK1 therapies, such as upadacitinib. Upadacitinib is a selective and reversible JAK inhibitor approved for treating UC; RA; psoriatic arthritis; ankylosing spondylitis (AS); and atopic dermatitis, and approval for Crohn’s disease is expected in the near future. This review intends to describe the mechanism of upadacitinib, evaluate the current clinical evidence of its effectiveness in treating IBD, and discuss safety considerations.
References
Abraham C, Medzhitov R. Interactions between the host innate immune system and microbes in inflammatory bowel disease. Gastroenterol. 2011;140(6):1729-1737. DOI: https://doi.org/10.1053/j.gastro.2011.02.012
Garrett WS, Gordon JI, Glimcher LH. Homeostasis and inflammation in the intestine. Cell. 2010;140(6): 859-870. DOI: https://doi.org/10.1016/j.cell.2010.01.023
O’Shea JJ, Plenge R. JAK and STAT signaling molecules in immunoregulation and immune-mediated disease. Immunity. 2012;36(4):542-550. DOI: https://doi.org/10.1016/j.immuni.2012.03.014
Sandborn WJ, Su C, Sands BE, et al. Tofacitinib as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2017; 376(18):1723-1736. DOI: https://doi.org/10.1056/NEJMoa1606910
FDA News Release. FDA approves new treatment for moderately to severely active ulcerative colitis. May 30, 2018. https://www.fda.gov/news-events/press-announcements/fda-approves-new-treatment-moderately-severely-active-ulcerative-colitis. Accessed July 25, 2023.
FDA Safety Announcement. FDA approves Boxed Warning about increased risk of blood clots and death with higher dose of arthritis and ulcerative colitis medicine tofacitinib (Xeljanz, Xeljanz XR). Feb. 4, 2021.
FDA Safety Announcement. Initial safety trial results find increased risk of serious heart related problems and cancer with arthritis and ulcerative colitis medicine Xeljanz, Xeljanz XR (tofacitinib). Feb. 4, 2021. https://www.fda.gov/drugs/drug-safety-and-availability/initial-safety-trial-results-find-increased-risk-serious-heart-related-problems-and-cancer-arthritis. Accessed July 25, 2023.
Ma C, Jairath V, Vande Casteele N. Pharmacology, efficacy and safety of JAK inhibitors in Crohn’s disease. Best Pract Res Clin Gastroenterol. 2019;38-39:101606. DOI: https://doi.org/10.1016/j.bpg.2019.03.002
Makurvet FD. Biologics vs. small molecules: Drug costs and patient access. Med Drug Discov. 2020 Nov;9:100075. DOI: https://doi.org/10.1016/j.medidd.2020.100075
Clementi ME, Marini S, Condo SG, et al. Antibodies against small molecules. Ann Ist Super Sanita. 1991;27(1):139-143.
Bousoik E, Montazeri Aliabadi H. “Do we know jack about JAK?” A closer look at JAK/STAT signaling pathway. Front Oncol. 2018 Jul 31;8:287. DOI: https://doi.org/10.3389/fonc.2018.00287
Cordes F, Foell D, Ding JN, et al. Differential regulation of JAK/STAT-signaling in patients with ulcerative colitis and Crohn’s disease. World J Gastroenterol. 2020;26(28):4055-4075. DOI: https://doi.org/10.3748/wjg.v26.i28.4055
Kohlhuber F, Rogers NC, Watling D, et al. A JAK1/JAK2 chimera can sustain alpha and gamma interferon responses. Mol Cell Biol. 1997;17(2):695-706. DOI: https://doi.org/10.1128/MCB.17.2.695
Velazquez L, Fellous M, Stark GR, et al. A protein tyrosine kinase in the interferon alpha/beta signaling pathway. Cell. 1992;70(2):313-322. DOI: https://doi.org/10.1016/0092-8674(92)90105-L
Ihle JN, Witthuhn BA, Quelle FW, et al. Signaling through the hematopoietic cytokine receptors. Ann Rev Immunol. 1995;13(1):369-398. DOI: https://doi.org/10.1146/annurev.iy.13.040195.002101
Guschin D, Rogers N, Briscoe J, et al. A major role for the protein tyrosine kinase JAK1 in the JAK/STAT signal transduction pathway in response to interleukin-6. EMBO J. 1995;14(7):1421-1429. DOI: https://doi.org/10.1002/j.1460-2075.1995.tb07128.x
Yamaoka K. Janus kinase inhibitors for rheumatoid arthritis. Curr Opin Chem Biol. 2016;32:29-33. DOI: https://doi.org/10.1016/j.cbpa.2016.03.006
Clark JD, Flanagan ME, Telliez JB. Discovery and development of Janus kinase (JAK) inhibitors for inflammatory diseases. J Med Chem. 2014;57(12):5023–5038. DOI: https://doi.org/10.1021/jm401490p
Danese S, Vermeire S, Zhou W, et al. Upadacitinib as induction and maintenance therapy for moderately to severely active ulcerative colitis: results from three phase 3, multicentre, double-blind, randomized trials. Lancet. 2022;399(10341):2113-2128. DOI: https://doi.org/10.1016/S0140-6736(22)00581-5
Loftus Jr EV, Panés J, Lacerda AP, et al. Upadacitinib induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2023;388(21):1966-1980. DOI: https://doi.org/10.1056/NEJMoa2212728
Coskun M, Salem M, Pedersen J, et al. Involvement of JAK/STAT signaling in the pathogenesis of inflammatory bowel disease. Pharmcol Res. 2013;76:1-8. DOI: https://doi.org/10.1016/j.phrs.2013.06.007
Ytterberg SR, Bhatt DL, Mikuls TR, et al. Cardiovascular and cancer risk with tofacitinib in rheumatoid arthritis. N Engl J Med. 2022;386(4):316-326. DOI: https://doi.org/10.1056/NEJMoa2109927
Balanescu AR, Citera G, Pascual-Ramos V, et al. Infections in patients with rheumatoid arthritis receiving tofacitinib versus tumour necrosis factor inhibitors: results from the open-label, randomized control ORAL Surveillance trial. Ann Rheum Dis. 2022;81:1491-1503. DOI: https://doi.org/10.1136/ard-2022-222405
Fleischmann R, Mysler E, Bessette L, et al. Long-term safety and efficacy of upadacitinib or Adalimumab in patients with rheumatoid arthritis: results through 3 years from the SELECT-COMPARE study. RMD Open. 2022;8(1):1-12. DOI: https://doi.org/10.1136/rmdopen-2021-002012
Mosli MH, Feagan BG, Sandborn WJ. Histologic evaluation of ulcerative colitis: a systematic review of disease activity indices. Inflamm Bowel Dis. 2014;20(3):564-575. DOI: https://doi.org/10.1097/01.MIB.0000437986.00190.71
Geboes K, Riddell R, Oct a, et al. A reproducible grading scale for histological assessment of inflammation in ulcerative colitis. Gut. 2004;47(3):404-409. DOI: https://doi.org/10.1136/gut.47.3.404
Vermeire S, Tanida S, Hu R. S856 Efficacy of upadacitinib induction therapy in patients with moderately to severely active ulcerative colitis by biologic inadequate responder status: results from two randomized Phase 3 studies. Am J Gastroenterol. 2021;116(1):S399-S400. DOI: https://doi.org/10.14309/01.ajg.0000776956.67877.43
Schreiber SW, Lim A, Lacerda AP. P630 Upadacitinib improves clinical outcomes in patients with moderate to severely active Crohn’s disease irrespective of previous failure to respond to biologics or conventional therapies. J Crohn’s Colitis. 2023;17(Supplement_1):i759-i762. DOI: https://doi.org/10.1093/ecco-jcc/jjac190.0760
Silverberg JI, de Bruin-Weller M, Bieber T, et al. Upadacitinib plus topical corticosteroids in atopic dermatitis: Week 52 AD Up study results. J Allerg Clin Immunol. 2022;149(3):977-987. DOI: https://doi.org/10.1016/j.jaci.2021.07.036
Simpson EL et al. Poster presented at: DERM 2021, August 5-8, 2021.
Cohen SB, Van Vollenhoven R, Curtis JR. POS0220 integrated safety profile of upadacitinib with up to 4.5 years of exposure in patients with rheumatoid arthritis. Ann Rheum Dis. 2021; 80(Suppl 1):328-329. DOI: https://doi.org/10.1136/annrheumdis-2021-eular.1856
Simpson EL, Silverberg JI, Nosbaum A. Integrated safety analysis of abrocitinib for the treatment of moderate-to-severe atopic dermatitis from the phase II and phase III clinical trial program. Am J Clin Derm. 2021;22(5):693-707. DOI: https://doi.org/10.1007/s40257-021-00618-3
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Canadian IBD Today

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.