Updates In The Management Of Pediatric Inflammatory Bowel Disease
DOI:
https://doi.org/10.58931/cibdt.2024.2126Abstract
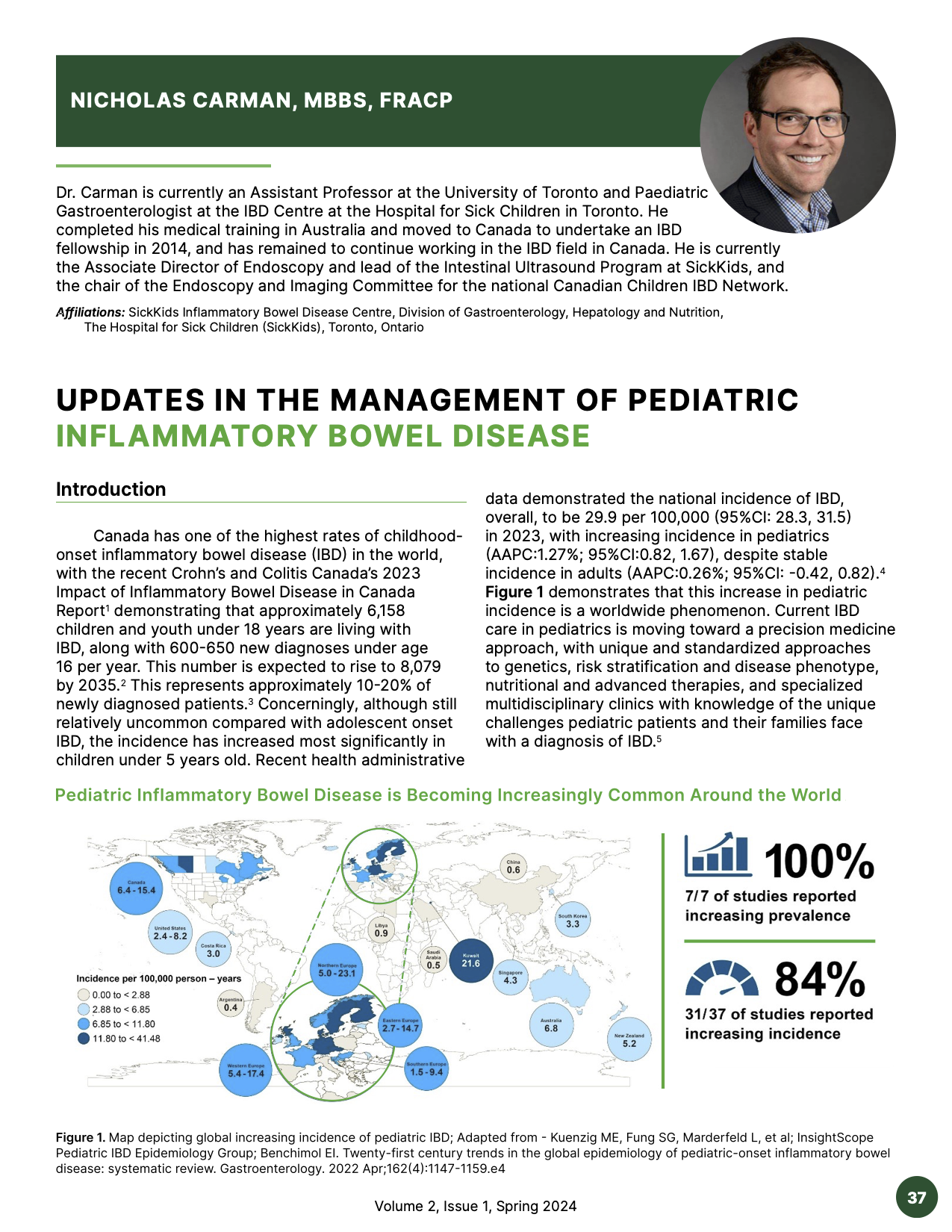
Canada has one of the highest rates of childhoodonset inflammatory bowel disease (IBD) in the world, with the recent Crohn’s and Colitis Canada’s 2023 Impact of Inflammatory Bowel Disease in Canada Report demonstrating that approximately 6,158 children and youth under 18 years are living with IBD, along with 600-650 new diagnoses under age 16 per year. This number is expected to rise to 8,079 by 2035. This represents approximately 10-20% of newly diagnosed patients. Concerningly, although still relatively uncommon compared with adolescent onset IBD, the incidence has increased most significantly in children under 5 years old. Recent health administrative data demonstrated the national incidence of IBD, overall, to be 29.9 per 100,000 (95%CI: 28.3, 31.5) in 2023, with increasing incidence in pediatrics (AAPC:1.27%; 95%CI:0.82, 1.67), despite stable incidence in adults (AAPC:0.26%; 95%CI: -0.42, 0.82). Figure 1 demonstrates that this increase in pediatric incidence is a worldwide phenomenon. Current IBD care in pediatrics is moving toward a precision medicine approach, with unique and standardized approaches to genetics, risk stratification and disease phenotype, nutritional and advanced therapies, and specialized multidisciplinary clinics with knowledge of the unique challenges pediatric patients and their families face with a diagnosis of IBD.
References
El-Matary W, Carroll MW, Deslandres C, et al. The 2023 impact of inflammatory bowel disease in Canada: special populations-children and adolescents with IBD. J Can 41 Volume 2, Issue 1, Spring 2024 Assoc Gastroenterol. 2023;6(Suppl 2):S35-s44. DOI: https://doi.org/10.1093/jcag/gwad016
Benchimol EI, Bernstein CN, Bitton A, C, et al. Trends in epidemiology of pediatric inflammatory bowel disease in Canada: distributed network analysis of multiple population-based provincial health administrative databases. Am J Gastroenterol. 2017;112(7):1120-34. DOI: https://doi.org/10.1038/ajg.2017.97
Benchimol EI, Manuel DG, Guttmann A, et al. Changing age
demographics of inflammatory bowel disease in Ontario, Canada: a population-based cohort study of epidemiology trends. Inflamm Bowel Dis. 2014;20(10):1761-9. DOI: https://doi.org/10.1097/MIB.0000000000000103
Coward S, Benchimol EI, Bernstein CN, et al. Forecasting the incidence and prevalence of inflammatory bowel disease: A Canadian nationwide analysis. Am J Gastroenterol. 2024. DOI: https://doi.org/10.14309/ajg.0000000000002687
Uhlig HH, Booth C, Cho J, et al. Precision medicine in monogenic inflammatory bowel disease: proposed mIBD REPORT standards. Nat Rev Gastroenterol Hepatol. 2023;20(12):810-28. DOI: https://doi.org/10.1038/s41575-023-00838-4
Sartor RB. Mechanisms of disease: pathogenesis of Crohn’s disease and ulcerative colitis. Nat Clin Pract Gastroenterol Hepatol. 2006;3(7):390-407. DOI: https://doi.org/10.1038/ncpgasthep0528
Muise AM, Snapper SB, Kugathasan S. The age of gene discovery in very early onset inflammatory bowel disease. Gastroenterology. 2012;143(2):285-8. DOI: https://doi.org/10.1053/j.gastro.2012.06.025
Nambu R, Warner N, Mulder DJ, et al. A systematic review of monogenic inflammatory bowel disease. Clin Gastroenterol Hepatol. 2022;20(4):e653-e63. DOI: https://doi.org/10.1016/j.cgh.2021.03.021
Gerasimidis K, Russell RK, Giachero F, et al. Precision nutrition in pediatric IBD: A position paper from the ESPGHAN special interest group for basic science and translational research, the IBD Porto group, and allied health professionals. JPGN. 2024;78(2):428-45. DOI: https://doi.org/10.1002/jpn3.12096
van Rheenen PF, Aloi M, Assa A, et al. The medical management of paediatric Crohn’s disease: an ECCOESPGHAN Guideline update. J Crohn’s Colitis. 2020 Oct 7:jjaa161.
Swaminath A, Feathers A, Ananthakrishnan AN, et al. Systematic review with meta-analysis: enteral nutrition therapy for the induction of remission in pediatric Crohn’s disease. AP & T. 2017;46(7):645-56. DOI: https://doi.org/10.1111/apt.14253
Hu D, Ren J, Wang G, et al. Exclusive enteral nutritional therapy can relieve inflammatory bowel stricture in Crohn’s disease. J Clin Gastroenterol. 2014;48(9):790-5. DOI: https://doi.org/10.1097/MCG.0000000000000041
Afzal NA, Davies S, Paintin M, et al. Colonic Crohn’s disease in children does not respond well to treatment with enteral nutrition if the ileum is not involved. Dig Dis Sci. 2005;50(8):1471-5. DOI: https://doi.org/10.1007/s10620-005-2864-6
Moriczi M, Pujol-Muncunill G, Martín-Masot R, et al. Predictors of response to exclusive enteral nutrition in newly diagnosed Crohn´s disease in children: PRESENCE Study from SEGHNP. Nutrients. 2020;12(4). DOI: https://doi.org/10.3390/nu12041012
Jones CMA, Connors J, Dunn KA, et al. Bacterial taxa and functions are predictive of sustained remission following exclusive enteral nutrition in pediatric Crohn’s disease. Inflamm Bowel Dis. 2020;26(7):1026-37. DOI: https://doi.org/10.1093/ibd/izaa001
Frivolt K, Schwerd T, Werkstetter KJ, et al. Repeated exclusive enteral nutrition in the treatment of pediatric Crohn’s disease: predictors of efficacy and outcome. AP & T. 2014;39(12):1398-407. DOI: https://doi.org/10.1111/apt.12770
Gerasimidis K, Godny L, Sigall-Boneh R, et al. Current
recommendations on the role of diet in the aetiology and management of IBD. Frontline gastroenterology. 2022;13(2):160-7. DOI: https://doi.org/10.1136/flgastro-2020-101429
Levine A, Wine E, Assa A, et al. Crohn’s disease exclusion diet plus partial enteral nutrition induces sustained
remission in a randomized controlled trial. Gastroenterol. 2019;157(2):440-50.e8. DOI: https://doi.org/10.1053/j.gastro.2019.04.021
Sigall Boneh R, Sarbagili Shabat C, Yanai H, et al. Dietary therapy with the Crohn’s disease exclusion diet is a successful strategy for induction of remission in children and adults failing biological therapy. J Crohn’s Colitis. 2017;11(10):1205-12. DOI: https://doi.org/10.1093/ecco-jcc/jjx071
Hyams JS, Davis Thomas S, Gotman N, et al. Clinical and biological predictors of response to standardised paediatric colitis therapy (PROTECT): a multicentre inception cohort study. The Lancet. 2019;393(10182):1708-20. DOI: https://doi.org/10.1016/S0140-6736(18)32592-3
Gisbert JP, Marín AC, McNicholl AG, et al. Systematic review with meta-analysis: the efficacy of a second anti-TNF in patients with inflammatory bowel disease whose previous anti-TNF treatment has failed. AP & T. 2015;41(7):613-23. DOI: https://doi.org/10.1111/apt.13083
Stallard L, Frost K, Frost N, et al. Body surface area-based dosing of infliximab is superior to standard weight-based dosing in children with very early onset inflammatory bowel disease. Gastro Hep Advances. 2024;3(2):215-20. DOI: https://doi.org/10.1016/j.gastha.2023.11.004
Assa A, Matar M, Turner D, et al. Proactive monitoring of adalimumab trough concentration associated with increased clinical remission in children with Crohn’s disease compared with reactive monitoring. Gastroenterology. 2019;157(4):985-96.e2. DOI: https://doi.org/10.1053/j.gastro.2019.06.003
Feagan BG, Rutgeerts P, Sands BE, et al. Vedolizumab as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2013;369(8):699-710. DOI: https://doi.org/10.1056/NEJMoa1215734
Atia O, Shavit-Brunschwig Z, Mould DR, et al. Outcomes, dosing, and predictors of vedolizumab treatment in children with inflammatory bowel disease (VEDOKIDS): a prospective, multicentre cohort study. Lancet Gastroenterol Hepatol. 2023;8(1):31-42. DOI: https://doi.org/10.1016/S2468-1253(22)00307-7
Rowland P, McNicol M, Kiel A, et al. Proactive therapeutic drug monitoring and vedolizumab dose optimization in children with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2024 Jan. 25. DOI: https://doi.org/10.1002/jpn3.12132
Sands BE, Sandborn WJ, Panaccione R, et al. Ustekinumab as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2019;381(13):1201-14. DOI: https://doi.org/10.1056/NEJMoa1900750
Feagan BG, Sandborn WJ, Gasink C, et al. Ustekinumab as induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2016;375(20):1946-60. DOI: https://doi.org/10.1056/NEJMoa1602773
Dhaliwal J, McKay HE, Deslandres C, et al. One-year outcomes with ustekinumab therapy in infliximab-refractory paediatric ulcerative colitis: a multicentre prospective study. AP & T. 2021;53(12):1300-8. DOI: https://doi.org/10.1111/apt.16388
Chavannes M, Martinez-Vinson C, Hart L, Ket al. Management of paediatric patients with medically refractory Crohn’s disease using ustekinumab: a multicentred cohort study. J Crohn’s Colitis. 2019;13(5):578-84. DOI: https://doi.org/10.1093/ecco-jcc/jjy206
Ricciuto A, McKay H, deBruyn J, et al. P512 Early proactive therapeutic drug monitoring with ustekinumab therapy in pediatric Crohn’s Disease. J Crohn’s Colitis. 2024;18(Supplement_1):i1012-i3. DOI: https://doi.org/10.1093/ecco-jcc/jjad212.0642
Sandborn WJ, Su C, Sands BE, et al. Tofacitinib as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2017;376(18):1723-36. DOI: https://doi.org/10.1056/NEJMoa1606910
Moore H, Dubes L, Fusillo S, et al. Tofacitinib therapy in children and young adults with pediatric-onset medically refractory inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2021;73(3):e57-e62. DOI: https://doi.org/10.1097/MPG.0000000000003190
Constant BD, Baldassano R, Kirsch J, et al. Tofacitinib salvage therapy for children hospitalized for corticosteroidand biologic-refractory ulcerative colities. J Pediatr Gastroenterol Nutr. 2022;75(6):724-30. DOI: https://doi.org/10.1097/MPG.0000000000003616
Spencer EA, Bergstein S, Dolinger M, et al. Single center experience with upadacitinib for refractory adolescent inflammatory bowel disease. NASPGHAN, San Diego 2023. DOI: https://doi.org/10.1093/ibd/izad300
Dolinger MT, Spencer EA, Lai J, et al. Dual biologic and small molecule therapy for the treatment of refractory pediatric inflammatory bowel disease. Inflamm Bowel Dis. 2021;27(8):1210-4. DOI: https://doi.org/10.1093/ibd/izaa277
Penagini F, Lonoce L, Abbattista L, et al. Dual biological therapy and small molecules in pediatric inflammatory bowel disease. Pharmacol Res. 2023;196:106935. DOI: https://doi.org/10.1016/j.phrs.2023.106935
Yerushalmy-Feler A, Olbjorn C, Kolho KL, et al. Dual biologic or small molecule therapy in refractory pediatric inflammatory bowel disease (DOUBLE-PIBD): A multicenter study from the pediatric IBD Porto Group of ESPGHAN. Inflamm Bowel Dis. 2024;30(2):159-66. DOI: https://doi.org/10.1093/ibd/izad064
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Canadian IBD Today

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.