Vaccine-Preventable Disease in IBD
Relevance, Guidelines, and Considerations for Implementation
DOI:
https://doi.org/10.58931/cibdt.2023.1215Abstract
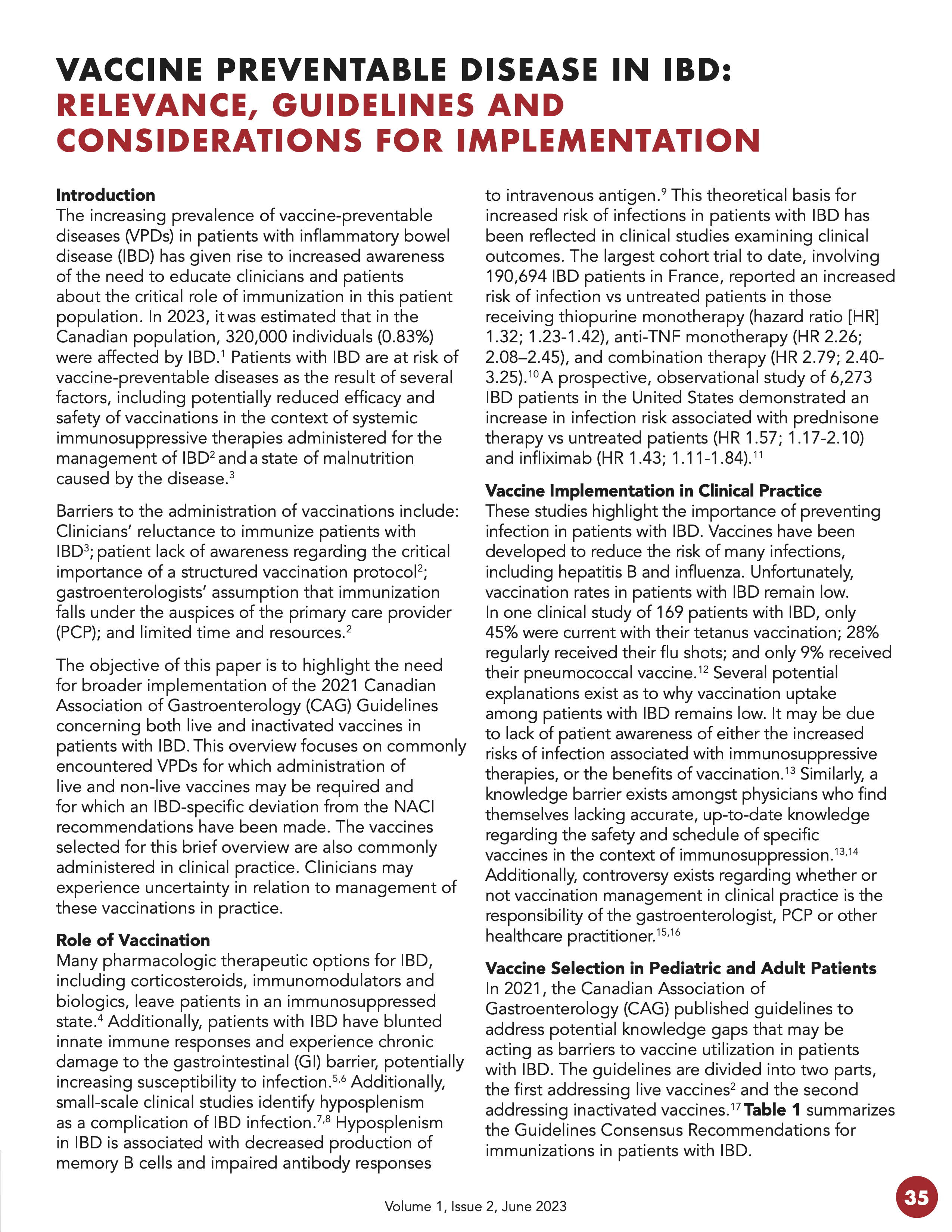
The increasing prevalence of vaccine-preventable diseases (VPDs) in patients with inflammatory bowel disease (IBD) has given rise to increased awareness of the need to educate clinicians and patients about the critical role of immunization in this patient population. In 2023, it was estimated that in the Canadian population, 320,000 individuals (0.83%) were affected by IBD. Patients with IBD are at risk of vaccine-preventable diseases as the result of several factors, including potentially reduced efficacy and safety of vaccinations in the context of systemic immunosuppressive therapies administered for the management of IBD2 and a state of malnutrition caused by the disease.
Barriers to the administration of vaccinations include: Clinicians’ reluctance to immunize patients with IBD; patient lack of awareness regarding the critical importance of a structured vaccination protocol; gastroenterologists’ assumption that immunization falls under the auspices of the primary care provider (PCP); and limited time and resources.
The objective of this paper is to highlight the need for broader implementation of the 2021 Canadian Association of Gastroenterology (CAG) Guidelines concerning both live and inactivated vaccines in patients with IBD. This overview focuses on commonly encountered VPDs for which administration of live and non-live vaccines may be required and for which an IBD-specific deviation from the NACI recommendations have been made. The vaccines selected for this brief overview are also commonly administered in clinical practice. Clinicians may experience uncertainty in relation to management of these vaccinations in practice.
References
Coward S, Benchimol EI, Bernstein C, Avina-Zubieta JA, Bitton A, Hracs L, Jones J, Kuenzig E, Lu L, Murthy SK, Nugent Z, Otley AR, Panaccione R, Pena-Sanchez JN, Singh H, Targownik LE, Windsor JW, Kaplan G. A35 Forecasting the incidence and prevalence of inflammatory bowel disease: A Canadian nation-wide analysis. J Can Assoc Gastroenterol. 2023 Mar 7;6(Suppl 1):19-20. doi:10.1093/jcag/gwac036.035 DOI: https://doi.org/10.1093/jcag/gwac036.035
Benchimol EI, Tse F, Carroll MW, deBruyn JC, McNeil SA, Pham-Huy A, et al. Canadian Association of Gastroenterology Clinical Practice Guideline for Immunizations in Patients With Inflammatory Bowel Disease (IBD)-Part 1: Live Vaccines. Gastroenterol. 2021 Aug;161(2):669-680. DOI: https://doi.org/10.1053/j.gastro.2020.12.079
Waszczuk K, Waszczuk E, Szenborn L. Can we better protect patients with inflammatory bowel disease against infections – patient attitude and personal immunization knowledge. Acta Gastro-Enterologica Belgica. 2018 April-June;81:257-261.
Murdaca, G, Spanò, F, Contatore, M, Guastalla, A, Penza, E, Magnani, et al. Infection risk associated with anti-TNF-α agents: a review. Expert Opinion on Drug Safety. 2015;14(4):571-582. DOI: https://doi.org/10.1517/14740338.2015.1009036
Marks DJB, Harbord MWN, Macallister R, Rahman FZ, Young J, Al-lazikani B, et al. Defective acute inflammation in Crohn’s disease: a clinical investigation. Lancet. 2006; 367:668-678. DOI: https://doi.org/10.1016/S0140-6736(06)68265-2
Casanova JL, Abel L. Revisiting Crohn’s disease as a primary immunodeficiency of macrophages: Figure 1. JEM. 2009;206(9):1839-1843. DOI: https://doi.org/10.1084/jem.20091683
Ryan FP, Smart RC, Holdsworth CD, Preston E. Hyposplenism in inflammatory bowel disease. Gut. 1978;19:50-55. DOI: https://doi.org/10.1136/gut.19.1.50
Rameh BS, Stevens F., McCarthy CF. Hyposplenism in inflammatory bowel disease. Ir J Med Sci.1988;157(1):8-9. DOI: https://doi.org/10.1007/BF02953677
Ryan F, Jones JV, Wright J K, Holdsworth CD. Impaired immunity in patients with inflammatory bowel disease and hyposplenism: the response to intravenous cpX 1 74. Gut.1981 Oct;22:187-189. DOI: https://doi.org/10.1136/gut.22.3.187
Kirchgesner J, Lemaitre M, Carrat F, Zureik M, Carbonnel F, Dray-Spira R. Risk of serious and opportunistic infections associated with treatment of inflammatory bowel diseases. Gastroenterology. 2018;155(2):337–346.e10. DOI: https://doi.org/10.1053/j.gastro.2018.04.012
Lichtenstein GR, Feagan BG, Cohen RD, Salzberg BA, Diamond RH, Price S, et al. Serious infection and mortality in patients with Crohn’s disease: more than 5 years of follow-up in the TREAT™ registry. Am J Gastroenterol. 2012 Sep;107(9):1409-1422. DOI: https://doi.org/10.1038/ajg.2012.218
Melmed GY, Ippoliti AF, Papadakis KA, et al. Patients with inflammatory bowel disease are at risk for vaccine-preventable illnesses. Am J Gastroenterol. 2006;101(8):1834-1840. DOI: https://doi.org/10.1111/j.1572-0241.2006.00646.x
Yeung JH, Goodman KJ, Fedorak RN. Inadequate knowledge of immunization guidelines: a missed opportunity for preventing infection in immunocompromised IBD patients. Inflamm Bowel Dis. 2012;18(1):34-40. DOI: https://doi.org/10.1002/ibd.21668
Wasan SK, Calderwood AH, Long MD, Kappelman MD, Sandler RS, Farraye FA. Immunization rates and vaccine beliefs among patients with inflammatory bowel disease: an opportunity for improvement. Inflamm Bowel Dis. 2014;20(2):246-250.
Selby L, Hoellein A, Wilson JF. Are primary care providers uncomfortable providing routine preventive care for inflammatory bowel disease patients? Dig Dis Sci. 2011;56(3):819-824. DOI: https://doi.org/10.1007/s10620-010-1329-8
Wasan SK, Coukos JA, Farraye FA. Vaccinating the inflammatory bowel disease patient: deficiencies in gastroenterologists’ knowledge. Inflamm Bowel Dis. 2011;17(12):2536-2540. DOI: https://doi.org/10.1002/ibd.21667
Jones JL, Tse F, Carroll MW, deBruyn JC, McNeil SA, Pham-Huy A, et al. Canadian Association of Gastroenterology Clinical Practice Guideline for Immunizations in Patients With Inflammatory Bowel Disease (IBD)-Part 2: Inactivated Vaccines. J Can Assoc Gastroenterol. 2021 Jul 29;4(4):e72-e91. DOI: https://doi.org/10.1093/jcag/gwab016
Kochar B, Herfarth HH. Vaccinations in patients with inflammatory bowel disease in the west. Inflamm Intest Dis. 2018;3:11-15. DOI: https://doi.org/10.1159/000491752
DeBruyn J, Fonseca K, Ghosh S, et al. Immunogenicity of influenza vaccine for patients with inflammatory bowel disease on maintenance infliximab therapy: A randomized trial. Inflamm Bowel Dis 2016;22(3):638-47. DOI: https://doi.org/10.1097/MIB.0000000000000615
Khan N, Patel D, Trivedi C, Shah Y, Lichtenstein G, Lewis J, Yang YX. Overall and comparative risk of herpes zoster with pharmacotherapy for inflammatory bowel diseases: a nationwide cohort study. Clinical Gastroenterology and Hepatology. 2018 Dec 1;16(12):1919-27. DOI: https://doi.org/10.1016/j.cgh.2017.12.052
Chang K, Lee HS, Kim YJ, Kim SO, Kim SH, Lee SH, Song EM, Hwang SW, Park SH, Yang DH, Ye BD. Increased risk of herpes zoster infection in patients with inflammatory bowel diseases in Korea. Clinical Gastroenterology and Hepatology. 2018 Dec 1;16(12):1928-36. DOI: https://doi.org/10.1016/j.cgh.2018.05.024
Long MD, Martin C, Sandler RS, Kappelman MD. Increased risk of herpes zoster among 108 604 patients with inflammatory bowel disease. Alimentary pharmacology & therapeutics. 2013 Feb;37(4):420-9. DOI: https://doi.org/10.1111/apt.12182
Marehbian J, Arrighi MH, Hass S, Tian H, Sandborn WJ. Adverse events associated with common therapy regimens for moderate-to-severe Crohn’s disease. Official Journal of the American College of Gastroenterology. 2009 Oct 1;104(10):2524-33. DOI: https://doi.org/10.1038/ajg.2009.322
Gupta G, Lautenbach E, Lewis JD. Incidence and risk factors for herpes zoster among patients with inflammatory bowel disease. Clinical Gastroenterology and Hepatology. 2006 Dec 1;4(12):1483-90. DOI: https://doi.org/10.1016/j.cgh.2006.09.019
Marra F, Lo E, Kalashnikov V, et al. Risk of herpes zoster in individuals on biologics, disease-modifying antirheumatic drugs, and/or corticosteroids for autoimmune diseases: A systematic review and meta-analysis. Oct 1 (Vol. 3, No. 4). Oxford University Press. DOI: https://doi.org/10.1093/ofid/ofw205
Nguyen DL, Nguyen ET, Bechtold ML. Effect of immunosuppressive therapies for the treatment of inflammatory bowel disease on response to routine vaccinations: A meta-analysis. Dig Dis Sci. 2015;60(8):2446-2453. DOI: https://doi.org/10.1007/s10620-015-3631-y
Murthy SK, Kuenzig ME, Windsor JW, Ghia JE, Griffiths AM, Panaccione R, et al. Crohn’s and Colitis Canada’s 2021 Impact of COVID-19 and Inflammatory Bowel Disease in Canada: COVID-19 Vaccines-Biology, Current Evidence and Recommendations. J Can Assoc Gastroenterol. 2021 Nov 5;4(Suppl 2):S54-S60. DOI: https://doi.org/10.1093/jcag/gwab033
Botwin GJ, Li D, Figueiredo J, Cheng S, Braun J, McGovern DPB, Melmed GY, et al. Adverse events after SARS-CoV-2 mRNA vaccination among patients with inflammatory bowel disease. Am J Gastroenterol. 2021 Aug;116(8):1746-51. doi:10.14309/ajg.0000000000001342 DOI: https://doi.org/10.1101/2021.03.30.21254607
Kennedy NA, Goodhand JR, Bewshea C, Nice R, Chee D, Lin S, et al. Contributors to the CLARITY IBD study. Anti-SARS-CoV-2 antibody responses are attenuated in patients with IBD treated with infliximab. Gut. 2021 May;70(5):865-875. DOI: https://doi.org/10.1136/gutjnl-2021-324388
Khan N, Mahmud N. Effectiveness of SARS-CoV-2 vaccination in a veterans affairs cohort of patients with inflammatory bowel disease with diverse exposure to immunosuppressive medications. Gastroenterology. 2021 Sep 1;161(3):827-36. DOI: https://doi.org/10.1053/j.gastro.2021.05.044
Alexander JL, Moran GW, Gaya DR, et al. Inflammatory Bowel Disease section of the British Society of Gastroenterology and the Inflammatory Bowel Disease Clinical Research Group. SARS-CoV-2 vaccination for patients with inflammatory bowel disease: A British Society of Gastroenterology Inflammatory Bowel Disease section and IBD Clinical Research Group position statement. Lancet Gastroenterol Hepatol 2021;6(3):218-224. DOI: https://doi.org/10.1016/S2468-1253(21)00024-8
Siegel CA, Melmed GY, McGovern DP, et al. International Organization for the Study of Inflammatory Bowel Disease (IOIBD). SARS-CoV-2 vaccination for patients with inflammatory bowel diseases: Recommendations from an international consensus meeting. Gut. 2021;70(4):635-40. DOI: https://doi.org/10.1136/gutjnl-2020-324000
Julsgaard M, Christensen LA, Gibson PR, et al. Concentrations of adalimumab and infliximab in mothers and newborns, and effects on infection. Gastroenterology 2016;151(1):110-9. DOI: https://doi.org/10.1053/j.gastro.2016.04.002
Duricova D, Dvorakova E, Hradsky O, et al. Safety of anti-TNF-alpha therapy during pregnancy on long-term outcome of exposed children: A controlled, multicenter observation. Inflamm Bowel Dis. 2019;25(4):789-96. DOI: https://doi.org/10.1093/ibd/izy294
Beaulieu DB, Ananthakrishnan AN, Martin C, et al. Use of biologic therapy by pregnant women with inflammatory bowel disease does not affect infant response to vaccines. Clin Gastroenterol Hepatol. 2018;16(1):99-105. DOI: https://doi.org/10.1016/j.cgh.2017.08.041
Bortlik M, Duricova D, Machkova N, et al. Impact of anti-tumor necrosis factor alpha antibodies administered to pregnant women with inflammatory bowel disease on long-term outcome of exposed children. Inflamm Bowel Dis. 2014;20(3):495-501. DOI: https://doi.org/10.1097/01.MIB.0000440984.86659.4f
Coyle D, Coyle K, Bettinger JA, et al. Cost effectiveness of infant vaccination for rotavirus in Canada. Can J Infect Dis Med Microbiol. 2012;23(2):71-7. DOI: https://doi.org/10.1155/2012/327054
Kotirum S, Vutipongsatorn N, Kongpakwattana K, et al. Global economic evaluations of rotavirus vaccines: A systematic review. Vaccine 2017;35(26):3364-86. DOI: https://doi.org/10.1016/j.vaccine.2017.04.051
Wasan SK, Calderwood AH, Long MD, Kappelman MD, Sandler RS, Farraye FA. Immunization rates and vaccine beliefs among patients with inflammatory bowel disease: an opportunity for improvement. Inflamm Bowel Dis. 2014 Feb;20(2):246-250. DOI: https://doi.org/10.1097/01.MIB.0000437737.68841.87
Zhou F, Robar J, Stewart M, Jones J. Implementation of national guidelines on the management of vaccine preventable disease in patients with inflammatory bowel disease: barriers and facilitators in clinical practice. Abstract accepted for poster presentation at Canadian Digestive Disease Week 2023. DOI: https://doi.org/10.1016/S0016-5085(23)02251-5
Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011 Apr 23;6:42. DOI: https://doi.org/10.1186/1748-5908-6-42
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Canadian IBD Today

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.